**I know. It’s not Wednesday and it hasn’t been 2 weeks since our last case. But, we had a really interesting patient come in last week and his timing was perfect with a recent health update sent by the Pennsylvania Department of Health dealing with emergency toxicology, so we’re going to tackle this update together. Don’t worry, there will still be another emergency cardiology case out next week. Ok, let’s jump in:**
“Hey we need some help with this admitted patient NOW!” you hear one of your nurses tell you.
You hustle over to her room and see a 23-year-old male in extremis. He is shaking, he’s dripping sweat, and looks very unwell. He tells you that everything hurts and he feels like he can’t breathe.
Your charge nurse, Shannon, comes over and catches you up. “This is Mr. Jones. He came in from the local substance abuse rehab facility. He has a history of fentanyl abuse and last used 6 hours ago. He states that his dealer gets his stash from Philadelphia. This is his second episode of this ‘shaking/sweating/can’t breathe’ thing. The first one happened when he was en-route to us. EMS gave him some valium and it seemed to relax those symptoms. The admitting team isn’t quite sure what’s going on with him. Since you’re going to ask, here is his ECG:”
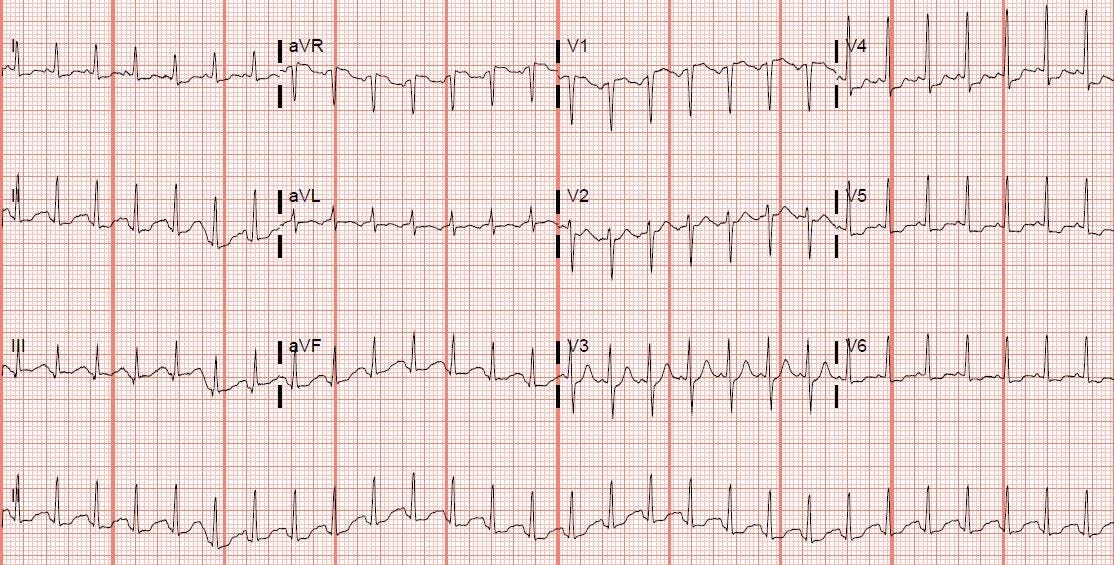
Rate: 160s
Rhythm: It’s challenging to see P waves in this ECG, but look closely at lead V2 and V3 and you can tease them out. This is sinus tachycardia, not SVT like I thought on first glance.
Axis: Normal
Intervals: Narrow QRS, normal PR, QTc looks ok too
Morphology: There’s some evidence of strain given the ST segment depression in V4/V5/V6 and the ST segment elevation in aVR
Final Read: This is Sinus Tachycardia with strain. This heart is beating too fast!
“Doc, take a look at the rest of his vitals!” You hear Shannon tell you as she notices you staring at the ECG too long (again).”
He’s tachycardic as high as the 190s, his blood pressure is 201/142 mmHg, O2 sat is 96% on 2L NC. He’s afebrile and blood sugar was 140 when checked upon arrival.
This is not good. His twitching/shaking is getting worse. It looks like he’s having rigid myoclonic jerks that could be confused as a seizure, but he’s talking to you the entire time (so it’s definitely not a seizure). He’s extremely anxious, diaphoretic, and vomiting. Something bad is going on, but what could it be?
[Please note, much of the following information comes from a Philadelphia Department of Public Health alert that can be found here and a report from the CDC found here. Much of this information is expert consensus and is not evidence based yet, because this is so new; this is also much more toxicology than my typical emergency cardiology case, but those of us in the northeastern region of the USA will definitely be seeing it soon, and it may be spreading to an ER near you, so please be on the lookout!]
It’s not uncommon for street drugs (such as fentanyl) to be cut (or mixed) with different substances. In the past several years, we’ve seen an increase in opioids being cut with xylazine (street name Tranq). Xylazine is an alpha-2 adrenergic receptor agonist and is traditionally used as a veterinary anesthetic. Xylazine will potentiate the lethality of opioids and can lead to fatal bradycardias. We’ve seen fentanyl and xylazine being mixed on the streets for the past few years (also called Tranq Dope) but this is something new.
Medetomidine is a synthetic alpha-2 agonists sedative that is 100-200x more potent than xylazine. From September 2024 to January 2025, 165 patients were hospitalized at different hospitals in Philadelphia for abnormal fentanyl withdrawal. Not only did these patients have the traditional symptoms (nausea, vomiting, sweating, agitation, etc.), they also had autonomic dysfunction, such as severe hypertension and tachycardia. Importantly, these patient’s symptoms were RESISENT to medications that had been classically used to treat fentanyl and xylazine overdoses. Testing showed that much of the fentanyl supply (>70%) in Philadelphia, PA is now being mixed with Medetomidine.
So what symptoms are we seeing and what is the timeline?
Medetomidine withdrawal starts abruptly withing hours of last use and progresses rapidly. It typically peaks between 18-36 hours after last use.
Symptoms include:
Tachycardia
Severe Hypertension
Nausea and Vomiting
Waxing and waning alertness
Anxiety
Severe diaphoresis
Restlessness
Tremor/Myoclonic jerks
How do we treat these patients?
Avoid PO medications (these patients are often having significant vomiting)
Initiate alpha-2 agonists EARLY (PA Dept of heath recommends Clonidine)
Treat the fentanyl withdrawal symptoms (PA Dept of heath recommends methadone)
These patients will need intensive monitoring (vital sign checks every hour, if not connected to continuous monitoring)
Check an ECG (my favorite part) and monitor for QTc prolongation
Treat anxiety and nausea/vomiting (PA Dept of heath recommends Olanzapine)
Treat their pain (PA Dept of heath recommends a combination of short acting opioids/ketamine/NSAIDS)
SOME OF THESE PATIENTS will require a dexmedetomidine drip in the ICU
More on this below
***WATCH OUT for concomitant medical problems (such as heart disease, COPD/Asthma, liver, psych disorders, etc) that can be exacerbated by the severe autonomic dysregulation***
***Please be aware, if you are a first responder responding to an overdose patient, when you give naloxone, check for BREATHING first, instead of responsiveness, as the patient may still be sedated from the medetomidine. THIS IS A CHANGE from a classic opioid-overdose response call (recommended by the PA dept of heath)***
Why Dexmedetomidine?
Great question. Dexmedetomidine (aka Precedex) is related to medetomidine. Prolonged exposure to dexmedetomidine can produce similar withdrawal symptoms as medetomidine and is traditionally reversed by a slow, controlled weening off of the drug. From the CDC’s recent brief on the initial 165 patients in Philadelphia, 137 (83%) were treated with and responded to Dexmedetomidine. Please be aware, of the 165 patients, 91% required ICU admission and 24% required intubation. Please be careful with these patients. Some come in looking like traditional fentanyl withdrawal, get admitted to the floor, and then crash. Involve your toxicology colleagues and addiction medicine colleagues early.
Case wrap up:
“SCOTT! I need some help in here, you call to your ER Pharmacist (why is he always on when I have crashing patients…). I need some clonidine and olanzapine, now!”
“I’ll let the ICU team know then need to come down and upgrade this patient from floor holding to ICU holding,” Shannon tells you. You, Scott, and the nursing team scramble to stabilize Mr. Jones’s blood pressure and heart rate. Just as you set up the dexmedetomidine drip, the ICU team comes down and takes over care.
Case Review:
Please be aware that there is a new drug (medetomidine) being cut with fentanyl causing severe and life-threatening withdrawal symptoms
The Pennsylvania Department of Heath and the CDC have put out several articles reviewing signs and symptoms of medetomidine withdrawal, which are linked below
Symptoms include traditional opioid withdrawal and AUTONOMIC INSTABILITY
Watch out for severe hypertension and tachycardia
Consider treating their symptoms with clonidine, olanzapine, and potentially a dexmedetomidine drip
Many of these patients will require an ICU admission
Involve your toxicology and addiction drug specialists early
Hit me up with any questions,
Lloyd
**Looking for a dynamic guest lecture on Emergency Cardiology for your Grand Rounds? Reach out here for a lecture request by Dr. Tannenbaum**
_________________________
Lloyd Tannenbaum, MD
APD, EM Residency
Geisinger Wyoming Valley




Just had a metetomidine OD (not withdrawal). Classic! Depressed LOC, resp depression, hypotensive, hyperglycemia, and bradycardia with HR of 27. Epi drip and into the ICU. Bad stuff.
Wow! Great info