Bonjour VTach!
Also, listen the first time Shannon tells you something...
“This is Medic 6 requesting stat medical command. Over.”
That’s not good. Medic 6 almost never calls for help. You and your charge nurse, Shannon, hustle over to the medical command phone, “Go ahead Medic 6, this is medical command.”
“Doc. We need your help. 56-year-old female coming in with severe chest pain. When we picked her up, she was diaphoretic, ashen, and looked bad. Actively puking as we got her into the rig. She looks like a cardiac case, but her ECG looks… not terrible? Maybe some ST depressions? Transmitting now, can you take a look, please? She’s also in and out of consciousness. I don’t have a good feeling about her.”
“Sure Medic 6, stand by.”
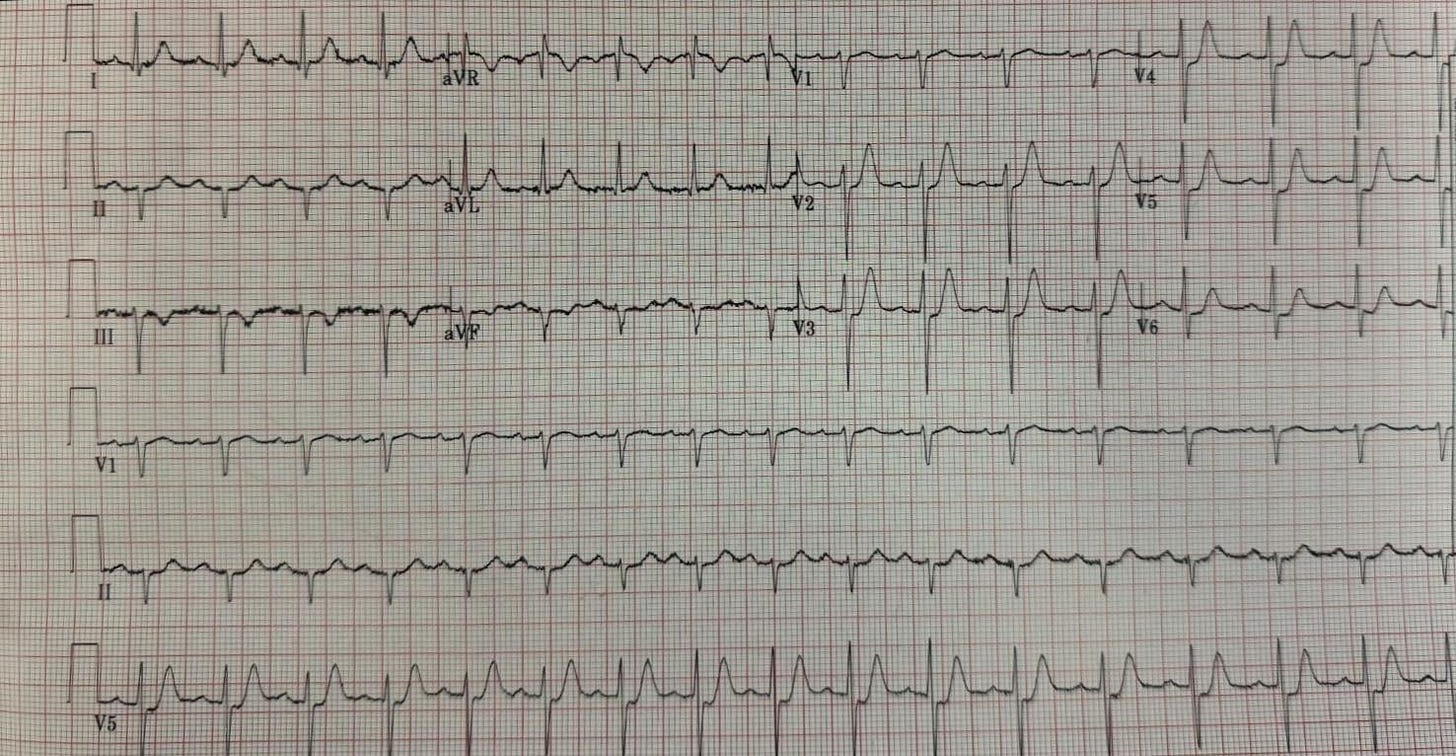
Rate: 115-ish
Rhythm: Normal sinus
Axis: Left axis deviation
Intervals: All pretty reasonable. PR looks ok, QRS is narrow, maybe a little shortening of the QTc but not terrible, probably related to rate.
Morphology: T waves look slightly sharper than normal. There is ST segment depression in the anterior leads, most notably V2 to V6. Slight ST segment elevation in aVR.
Final read: This is an ischemic ECG. The sharp T waves we’re seeing are concerning for early “Hyper-Acute T Waves” of ACS. This person needs a repeat ECG as soon as possible and a discussion with cardiology.
“Medic 6, this ECG is incredibly concerning for ischemia, great pick up. You have potentially hyperacute T waves and ST segment depressions in the anterior leads. I don’t think it’s a full “DeWinter’s Pattern” yet, but she needs a repeat ECG stat. How far out are you?”
“Hey Doc, we’re pulling in now. She still looks terrible. We’ve given her aspirin 325 mg, two tabs of nitro, 4 mg of morphine, and nothing is touching her. See you in a sec. Medic 6 out.”
“Sounds good Medic 6, please head directly to room 8 upon arrival. Hospital clear.”
“Shannon, who’s on for pharmacy today? We probably need the packet of STEMI meds.”
“Doc, I don’t know how you do it, but Scott is always on when you have a crashing patient. I’ll give him a heads up to meet you at bed 8… There’s the EMS door alarm, looks like Medic 6 is walking in. They’re moving fast. I’ll have him grab and RSI kit too, just in case.”
“Alert respiratory too, please. Hey guys, go ahead and give me the full report!”
“Doc, this is Mrs. O’Leary. 56-year-old female with severe chest pain and tightness. Says that she feels like there’s an elephant sitting on her chest. Was initially very vocal about her pain but it’s been getting worse and worse and her mental status is slipping. She’s in and out of consciousness for us. Most recent set of vitals show a heart rate in the 120s, BP 90/42, respiratory rate of 20, SpO2 of 95%, no fever, blood glucose 126. Moving her to your bed in 3 .. 2 .. 1. Good luck Doc, I’ll call you in about 30 for an update. We got a wreck on the highway to run off to.
“Thanks guys; Shannon, let’s get her hooked up to our monitors and get a repeat ECG, please.”
“Sounds good, Doc. Uhhh. Doc… Take a look at that tele monitor.”
“One sec, Shannon, I’m trying to help the tech set up for this repeat ECG.”
“NOW.” LOOK AT THE TELE MONITOR NOW,” you hear Shannon say in an incredibly stern tone that you haven’t heard before.
You look up, and this is what you see:
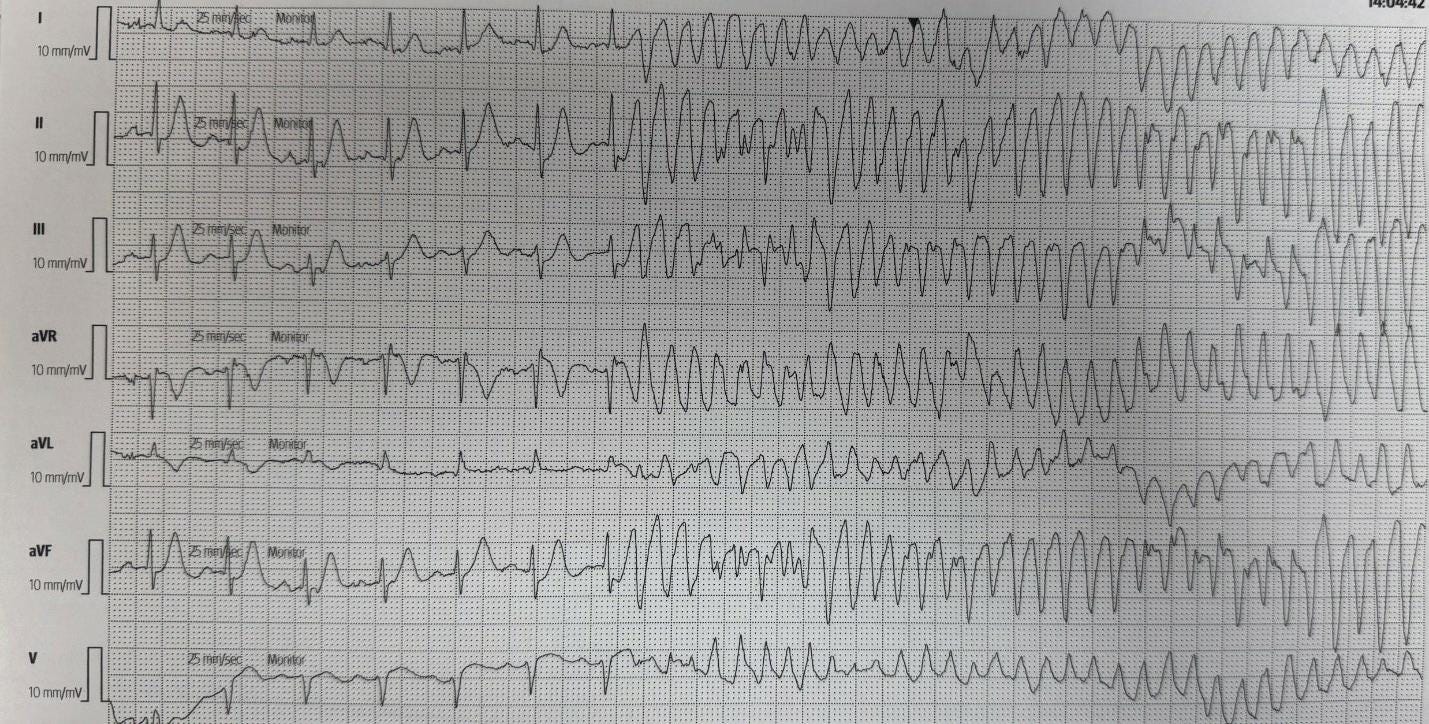
Rate: Initially around 115, then rates over 250
Rhythm: Initially organized and sinus, then definitely not sinus
Axis: Arguably not helpful right now
Intervals: Initially look ok, narrow QRS, reasonable PR, QTc looks ok, then definitely not ok, Wide complex QRS, loss of obvious P wave
Morphology: Initially can see the ST segment elevation in aVR still, then we transition to a wide complex tachycardia with fusion beats present.
Final read: Initially sinus rhythm and then the patient goes into a wide complex tachycardia. All of the beats don’t look the same, so this is not monomorphic VT. There are some larger complexes and then smaller complexes and then larger again. Is this the “twisting of the points” seen in torsades de pointes (TdP)? Or just good ol’ fashioned polymorphic Vtach? Is there a difference?
*******************************
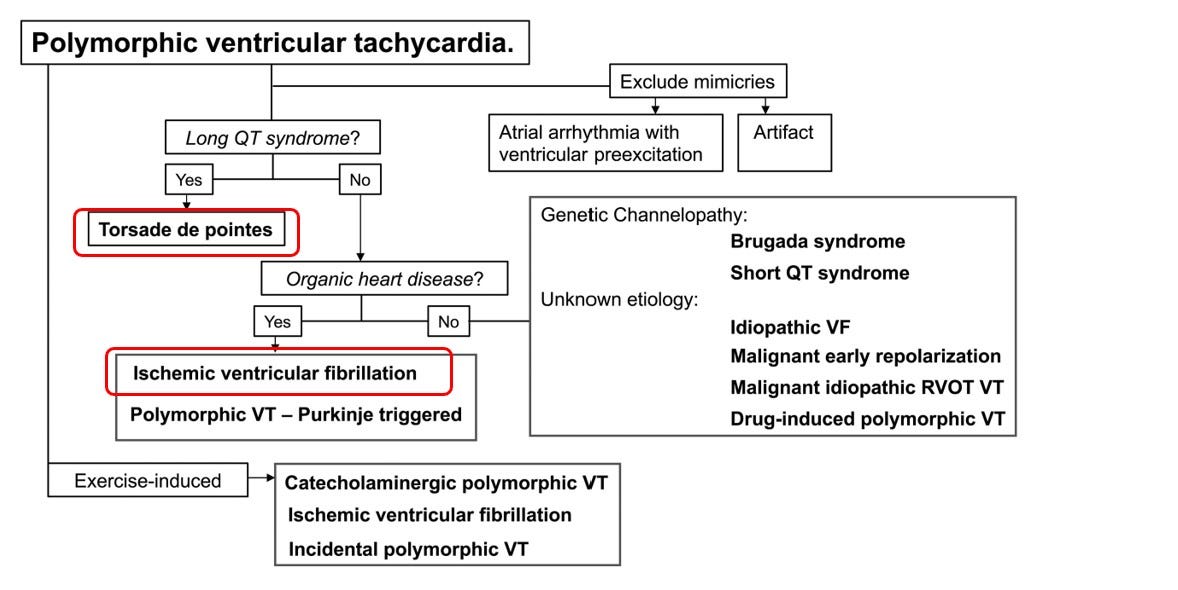
Let’s start with the basics on polymorphic ventricular tachycardia (PVT). Please note, much of this information comes from the AHA Journal, Circulation, which published a great review article on PVT which can be found here. Yes, there is a difference between TdP and PVT. All TdP is a form of PVT, but there are types of PVT that aren’t TdP. If that sounds super confusing, think of it as rectangles and squares. Remember, all squares (TdP in this analogy) are rectangles (PVT), but not all rectangles (PVT) are squares (TdP). But how do we tell the difference?
Your guide here is the QT interval and the patient’s presentation. The article from Circulation, referenced above, has a great flowchart that breaks down the different types of PVT, which is shown below. We’re only going to focus on two types, TdP and ischemic PVT/VF, which I boxed in red.
Ref: https://www.ahajournals.org/doi/epub/10.1161/CIRCULATIONAHA.121.055783
The term “Torsades de Pointes” was first used in 1969 by a French cardiologist, Dr. Dessertenne describing a certain type of PVT that occurred in patients with Long QT Syndrome. Here is a link to his paper, but it’s completely in French, so I’m not really sure what it says. My French is pas bon.
Luckily, the Circulation article is in English. It makes a point of calling out that Long QT Syndrome occurs when there are issues with the ion channels in the myocardium. This leads to an imbalance of electrolytes and can predispose patients to ventricular arrhythmias.
The formal diagnosis of TdP requires, according to the Circulation paper:
The likelihood that one of the congenital or acquired forms of long QT syndrome is present
The QT interval during sinus rhythm is prolonged
The arrhythmia has a characteristic mode of onset*
*What does point 3 mean? The Circulation article has a lot of words, but, what I think they’re trying to say is that it’s usually the R on T phenomenon that sets off the TdP. We’ll touch more on the R on T phenomenon next time, it’s pretty cool.
So, if we had to sum up TdP, we’d say that it’s a form of PVT that requires a prolonged QT interval and is usually set off by the R on T phenomenon.
But what about Mrs. O’leary? Her QTc wasn’t prolonged. What set off her PVT?
The other type of PVT I’d like to touch on is ischemic PVT/VF. It’s paired with ventricular fibrillation (VF) because when ischemia is the cause of PVT, it often, quickly, degrades into VF. To qualify for “ischemic PVT” the patient needs to develop this heart arrhythmia during an obvious time of myocardial ischemia. It may be during a stress test or it may be in the ER when they present for their MI. This is what you’ll see in the movies when someone just drops “dead of a heart attack.”
Formal diagnosis of ischemic PVT/VF requires the patient to have a run of polymorphic ventricular tachycardia or VF while having ACS. Remember, the patient does NOT need to be having a STEMI, this can be seen in NSTEMI patients too.
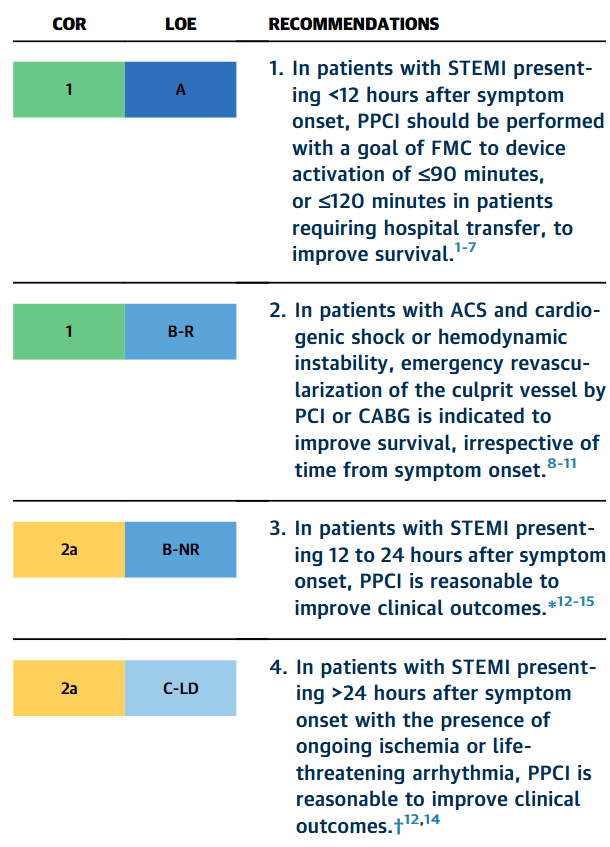
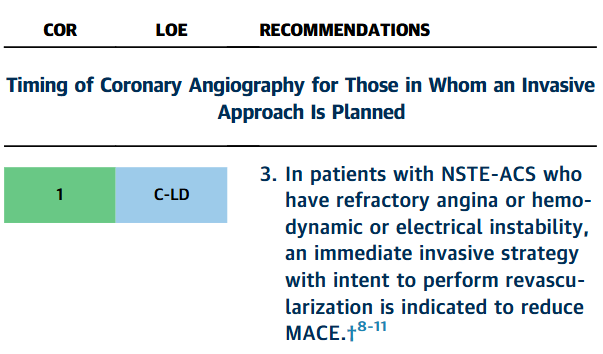
So, what do we do with these patients? In 2025, the ACC/AHA/ACEP/NAEMSP/SCAI Guidelines for the Management of Patients With ACS (link: https://www.jacc.org/doi/10.1016/j.jacc.2024.11.009) was published. There are two sections on electrically unstable patients with ACS that I’d like to highlight, but the short answer is, get them to a cath lab as soon as they’re stable enough. In the first chart, note that patients having a STEMI with >24 hours of symptoms AND electrical instability still benefit from an emergent cath. In the second chart, note that NSTEMI patients with electrical instability need an emergent cath, not an urgent cath.
Ref: https://www.jacc.org/doi/epdf/10.1016/j.jacc.2024.11.009
Ref: https://www.jacc.org/doi/epdf/10.1016/j.jacc.2024.11.009
Side note, there was a study that looked at keeping the patient strapped to a mechanical CPR device and taking them to the cath lab, but survival was terrible.
Ok, let’s sum up ischemic PVT/VF. Usually seen in patients having some form of acute coronary syndrome. Often very unstable and needs a cath lab as soon as possible, assuming you’re able to get them stabilized.
*********************
“HEY DOC! What’s the plan for Mrs. O’Leary? Did you notice the rhythm change on the telemetry?” If you keep standing there, Scott is going to run you over with the crash cart…
“Yes! Thank you! You’re right, this is bad. Mrs. O’Leary is in polymorphic VTach, likely due to her ongoing cardiac ischemia. She needs a cath NOW! Shannon, can you see if she’s responsive while I get the pads on her? We need to shock her as soon as possible.”
“Doc, GCS is 3, she’s not moving at all. I’m also having a lot of trouble finding a pulse. Starting CPR.”
“Got it, thanks Shannon. Scott, I need some epi please. Can you push that while I alert the cath lab and get them on standby. Everyone hold on, the Zoll is ready, shocking in 3… 2.. 1… everyone clear! Ok, resume CPR and let’s get that epi in. Let’s see if we can get her stable enough to get her upstairs. Hello? Interventional cardiology? I have a patient for you …”
Case wrap up:
Not all polymorphic Vtach is torsades de pointes, but torsades de pointes is a form of PVT.
Diagnosis of TdP requires a prolonged QT interval before the patient goes into PVT
Ischemia can also cause PVT
The entire spectrum of ACS can cause PVT, not just a STEMI
These patients need revascularization as soon as they are stable enough to make the transport to the cath lab
Hit me up with any questions,
Lloyd
**Looking for a dynamic guest lecture on Emergency Cardiology for your Grand Rounds? Reach out here for a lecture request by Dr. Tannenbaum. If you have reached out already, I have emailed you back. If you haven’t gotten it, please message me directly on Substack or just reply to this email.**
_________________________
Lloyd Tannenbaum, MD
APD, EM Residency
Geisinger Wyoming Valley


What a great class, Doc! I am a Brazilian medical student( 5th out of 6 years) who wants to be a cardiologis. Your publications help me to keep constantly in touch with cases of cardiology. Thanks you for that!!!