“IT’S HAPPENING AGAIN!!! HELP! HELP! I NEED A DOCTOR!!!!! I’M DYING!”
Well. That’s not a good start to a shift. You and your nursing teams run into the patient’s room to see a 56 year old male who actually doesn’t look that terrible? In fact, he doesn’t look like he’s dying at all. He’s definitely short of breath, but otherwise seems ok? Between gasps for breath, he tells you that he had a heart attack 12 days ago and this morning his chest felt “weird.” He then got very short of breath and drove himself to the hospital. Now he’s having the same pain as last time and is convinced he’s dying.
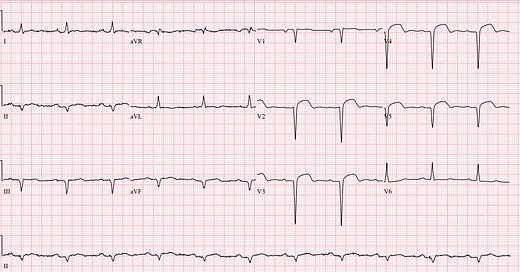
What a dramatic start to a shift! The tech hands you the patient’s EKG from today, let’s take a look while the nursing staff calms him down and gets his vital signs:
Rate: 68 ish
Rhythm: Looks sinus, there is a P before each QRS complex, the P is upright in lead II
Axis: Left axis
Intervals: Narrow QRS, maybe a slightly prolonged PR interval, QTc looks ok
Morphology: Yikes. There are some dome shaped ST segment elevation present in leads V2-V5, but there are no reciprocal changes.
Final read: It’s sure concerning for an anterior STEMI! There is ST segment elevation in V2 to V5.
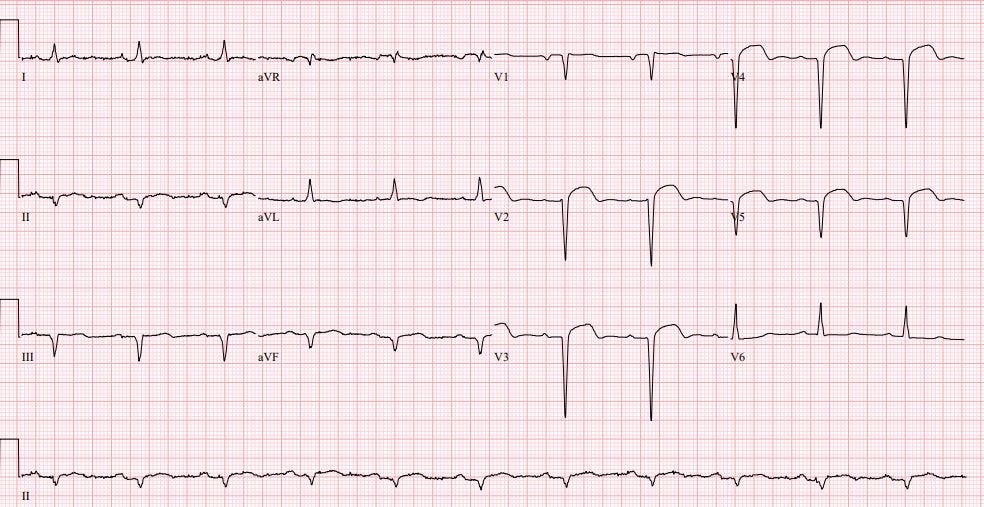
It looks bad right? Remember, between yells that he was 100% definitely dying, the patient told you he just had a heart attack a week and a half ago. And since we live in a magical world where medical records from outside hospitals are always available, you happen to have access to the other hospital's records where he had a GIGANTIC STEMI 12 days ago. Let’s take a look:
Rate: 72 ish
Rhythm: Sinus rhythm
Axis: Normal
Intervals: They all seems pretty reasonable. Narrow QRS, normal QTc.
Morphology: Wow. ST segment elevation in V1-V4
Final Read: This is an impressive anterior STEMI.
Terrifying right? I'll wait a second while you pick up your jaw from the floor. Now that's a STEMI. Even my 6 year old knows it. (We start EKG teaching at a young age in my house).
Well shoot. Now what. Is our patient still having a STEMI? Is it a 12 day long stemi? Is that ST segment elevation expected after an MI? How long does it last? Do we activate the cath lab? Do we just pretend that Dr. Willner is the attending and I go get another cup of tea?
Before diving into these questions, let’s take 30 seconds and review expected ST segment changes in patients having an acute myocardial infarction.
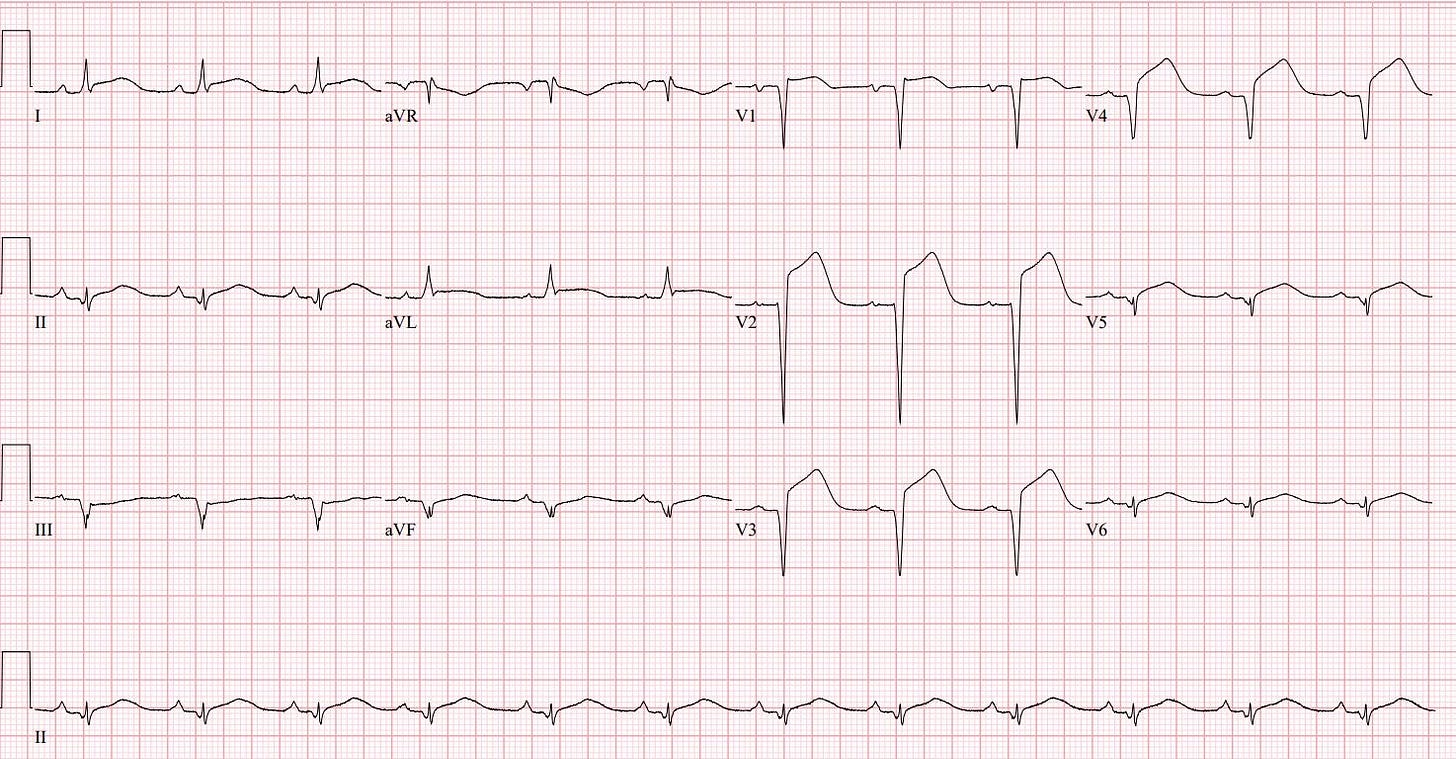
This first image below is one of the best examples of hyperacute T waves that I could find. It came from one of my mentors who taught me how to read ECGs. Notice how the ST segments are blended directly into the T wave at almost a 90 degree angle. These ST-T waves look like rockets about to take off. They are one of the earliest signs of an acute MI, occurring minutes to hours after acute coronary occlusion. Often, patients don’t come to the ER in time to catch these on ECG. Take a look:
Ok, so we missed the hyperacute T waves, what’s next?
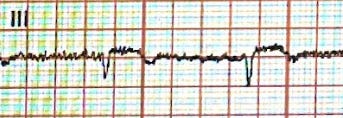
This next section comes from an inferior MI. You can see the ST segment elevation in III and aVF. Notice here that we have significant ST segment elevation. This will occur within the first few hours of acute coronary occlusion:
Ok, now take a look at lead III. Notice that the ST segments are still elevated but pathologic Q waves have started to form. Q waves will start to develop a few hours later. They are a marker of abnormal conduction and the beginning of myocardial scar formation:
Over time, you’ll see the ST segment begin to lower and the T waves will now be inverted. It usually takes 2-5 days for these changes to occur:
But when do the ST segments come back to baseline? Well, it usually takes about 2 weeks for the ST segment to normalize. And just to make things even less fair, in up to 60% of anterior MIs there is usually some degree of persistent ST segment elevation that just kind of hangs out on that patient’s EKG. So, did that help? Is this guy having a STEMI?
Luckily, my friend Kevin Kucharski, ultrasound guru, happened to be around and stopped by to help. We got this image on POCUS:
Well. I'm still really not very good at US. But even I can tell that's a giant LV. But, before the big reveal, take a look at what happens when Kevin put on the color flow:
Is there color moving across the septum? Is that normal? Am I just really bad at US?
Yes. No. Yes.
But, in this case, our patient has an LV aneurysm AND a septal rupture. That's right. He had such a massive STEMI 12 days ago that it caused severe heart damage and he ruptured his septum. Not good. But also not a STEMI. And remember, LV Aneurysms can cause persistent ST Segment elevation. Which is what is going on here. He will have that ST segment elevation likely forever, until CT surgery fixes the aneurysm. This is a patient who needs to carry a copy of his baseline EKG around with him or he will have a CODE STEMI called on him every time he comes to the ER.
Let's wrap up by circling back to our original questions:
Is our gentleman still having another STEMI? No
Is it a 12 day long STEMI? Still No
Is that ST segment elevation expected after an MI? It can be.
How long does ST segment elevation last after an MI? Up to 2 weeks
Do we activate the cath lab? I didn’t, but I did call cards right away and ask for help
What happened? The patient had a left ventricular aneurysm and a septal rupture
Do we just pretend that Dr. Willner is the attending and I go get another cup of tea? The thought did cross my mind…
Hit me up with any questions,
Lloyd
**Looking for a dynamic guest lecture on Emergency Cardiology for your Grand Rounds? Reach out here for a lecture request by Dr. Tannenbaum**
_________________________
Lloyd Tannenbaum, MD
APD, EM Residency
Geisinger Wyoming Valley
**I’ll be lecturing in Montreal with Dr. Amal Mattu and several other friends at the Emergency Cardiology Preconference for the International Conference on Emergency Medicine in May, come say hi!**








Great teaching. I love your prolific style of MedEd. And do you really eat EKG for breakfast in your house?
Wow. I'm a cardiac tech student in South Africa and I've seen a lot of STEMIs but this case was quite interesting!