“This is Medic 1015 requesting medical command stat, University of Kentucky do you copy?”
Uh oh. That’s not good. You hustle over to the radio and see your charge nurse walk over to listen in. “Go ahead medic 1015, medical command here!”
“Hey Doc, we have a little situation here. We were called out to a combative 30-something year old who was clearly high on something. According to bystanders, he has a complex psych and substance abuse history. We were unable to verbally de-escalate the situation, so, following protocol, we gave him IM droperidol and he calmed down real quick. Maybe a little too quick actually. After the droperidol, he went into some kind of weird rhythm and is now in cardiac arrest. We are starting ACLS and will be at your facility in 3-ish minutes. Medic 1015 out.”
You and the charge nurse look at each other. “Damn I wish they would have led with ‘WE HAVE A PATIENT IN CARDIAC ARREST!’ But, so be it. Let’s get the code cart ready and bring over the team. We have probably 120 seconds before arrival, let’s get ready to go.”
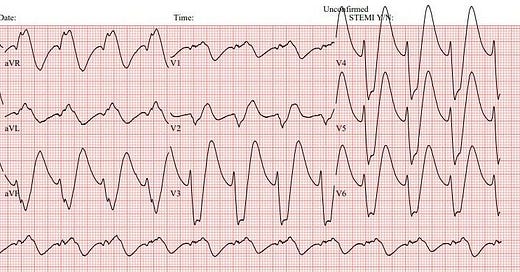
EMS arrives with the patient, still in full arrest. “Hey Doc! Pretty much no change from when we talked 2 minutes ago. He’s 2 rounds of ACLS in, last Epi was 1 minute ago. No pulse on last check. Here’s what his rhythm was doing before he arrested,” and he hands you a rhythm strip:
Yikes! That’s not good! You look back, make eye contact with your clinical pharmacist and look at each other with a knowing smile, “SCOTT! I need…”
“Bicarb!” you say at the same time “Lloyd, here’s 2 amps from the crash cart, let me run back to the pyxis and I’ll get a bunch more and prep a bicarb drip for you. One sec.”
“Ok, cool! Scott, I’ll just pontificate on how you knew I needed bicarb for a sec while you sprint to the pyxis.” What did we hear in the history and see in the rhythm strip that pushed us towards fixing this patient with bicarb?
This strip shows a really really really wide complex rhythm. To the point that the QRS complexes look goofy. They are so stretched out, it’s hard to really know what’s going on. In a patient like this, there are two categories that the pathology likely falls into. One is toxicology and the other is a severe electrolyte derangement. In an undifferentiated patient with this rhythm, you would want to consider giving two medications:
1) Calcium
2) Bicarb
Why? Well, let’s say it’s hyperkalemia and the patient’s potassium is 9. And that is what is causing the QRS complexes to stretch out. You’d give calcium (board answer is still to stabilize the cardiac membranes, although that is being called into question by some recent papers) and Bicarb as part of your hyperkalemia cocktail
Let’s say it’s toxicology. And you have poisoned sodium channels. You’d give sodium bicarb to overcome that blockade, which works by two different mechanisms, which we’ll address below. Oh, and the calcium? It’s not going to hurt the patient. It may even make their bones a little stronger. Oh, hey! The nurses are trying to get our attention.
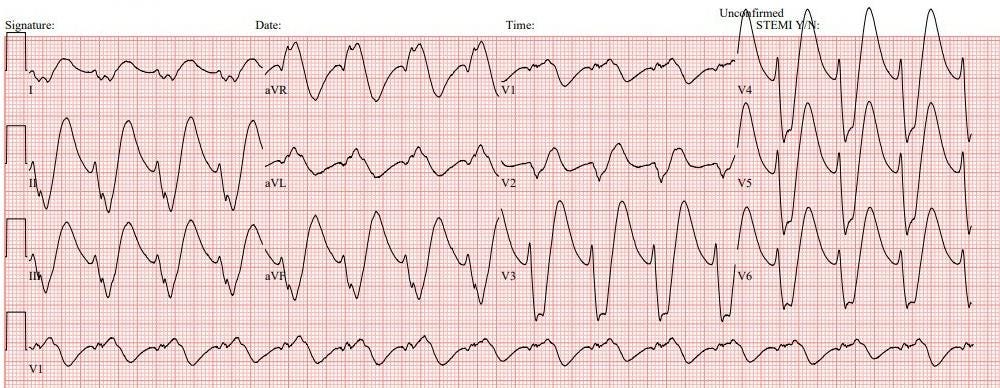
Woah! While we were pontificating, we got ROSC! Here’s his immediate post ROSC ECG:
Rate: right around 100 bpm
Rhythm: Not sinus
Axis: Probably extreme left, but you likely have more important things to focus on than axis right now
Intervals: the QRS is still insanely wide. >200msec.
Morphology: This doesn’t look good. We’re not at sinusoidal yet, but we will be soon if we don’t do something quick.
Final read: This is an extremely wide complex tachycardia concerning for a sodium channel blockade or severe electrolyte derangement
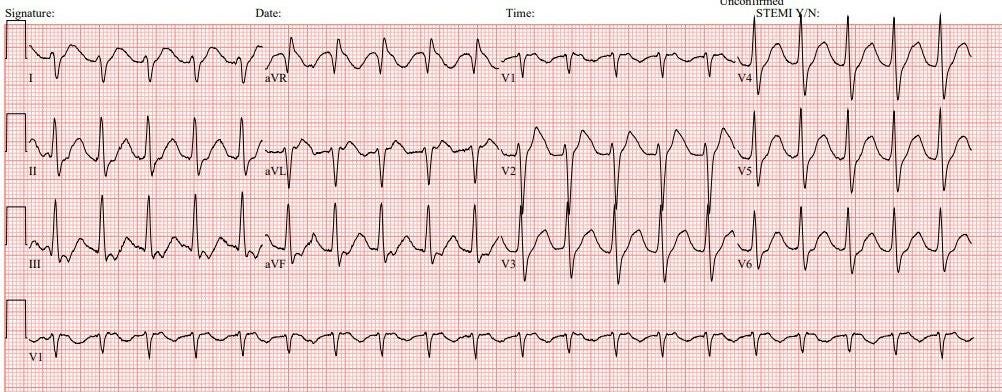
“Scott! Where are you with that… OH! You’re back. And you’re giving me the bicarb and handing the nurse the drip to run. Well. Uhhhh.. Great job! Go Cats!” You push another 2 amps of bicarb and start the drip. Just a quick reminder for a bicarb drip, it’s 3 amps of bicarb in D5W, NOT Normal Saline; you need D5W so the solution is iso-osmolar. Here’s the patient’s ECG after the additional bicarb:
Rate: 120 ish
Rhythm: I’m going to guess we’re back in sinus rhythm, but it’s hard to be 100% confident I see P waves
Axis: Right axis
Intervals: QRS complexes are narrow again, QTc is prolonged
Morphology: Some nonspecific ST-T wave changes (like the ST depressions in the inferior leads), there is also a terminal, slurred R wave in aVR (more below)
Final Read: (likely) sinus tachycardia with signs of a sodium channel blockade, though it is improving from the post-ROSC ECG above
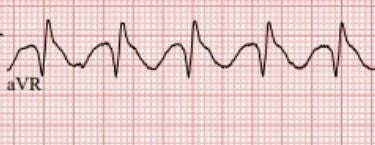
What is a terminal, slurred R wave in aVR? Let’s take a closer look:
See how the QRS complex just sort of ends at the R wave and then it slurs into the T wave? This used to be pathognomonic for a TCA overdose and would show up on board exams frequently. Since we’ve gotten away (mostly) from using TCAs, when you see this pattern, consider a Benadryl (diphenhydramine) overdose.
The ICU comes down to admit your patient. Luckily, the ICU attending is my friend and colleague, Dr. Alyssa Berns, who’s always willing to drop a little extra ICU knowledge as she admits your patient. “Dr. Berns, why does sodium bicarb work to overcome a sodium channel blockade?”
“Great question, Lloyd and Scott. Overdoses on sodium channel blocking medications poison the myocytes by blocking the fast sodium channels and prolonging the repolarization and refractory periods, which is the part of the cardiac cycle where bad things can happen (the heart is at high risk of ventricular arrhythmias). Giving extra sodium helps to overcome this by trying to overwhelm the receptors with sodium so that, even if many of them are blocked, there is plenty of sodium around, waiting for the opportunity to interact with the myocytes.
Why not just give sodium? We have lots of types of sodium and can even give 23% sodium in really special circumstances to raise sodium in certain clinical scenarios, such as patients who are trying to herniate. The reason is related to acid base status, the best part of medicine. Sodium channel blocking toxins that are floating around in the plasma are the ones that can wreak havoc, but if you cause an alkalosis, you can actually increase the amount of drug bound to plasma proteins and reduce the amount that is available to poison the heart. This is the reason that we start with sodium bicarb amps, which have high amounts of sodium, and then continue with a bicarb drip (which is nearly normonatremic and isosmolar) afterwards, to maintain a bit of alkalosis, and continue to supply sodium (the sodium content of an isotonic bicarb drip is 150mEq/L, which is slightly higher than physiologically normal levels).
How much sodium is an amp of bicarb? 50mEq in 50mL. There is also 50mEq of bicarb in there. This means that it is extremely concentrated and you can raise the sodium as much as 2mEq on the chemistry with one push!
So why don’t we use hypertonic saline? Well, it is rarely first line. The pH of saline solutions is below 6, no matter if we are talking about .9%, 2%, or 3%. If our goal by alkalinizing the sodium is to increase plasma protein binding of the drug, these solutions will do the opposite. That being said, there are case studies and animal models where hypertonic saline has been used successfully, and you can consider also that your patient is likely at the upper limit of tolerable alkalosis (above 7.50-7.55). While your critical patients can tolerate a remarkable level of acidosis, they cannot tolerate severe alkalosis.”
Thanks Dr. Berns! But what happened? Why did he arrest?
Great question. The patient presented with signs of a sodium blocker overdose. In this case, he had a known psych history (many psych meds will both prolong the QTc and widen the QRS), a history of substance abuse (opioids are sodium channel blockers), and was given droperidol (another potent sodium channel blocker) prehospital. All of these sodium channel blockers combined and caused his arrest.
Recap:
When you encounter an extremely wide complex tachycardia, reach for bicarb and calcium
A “Terminal Slurred R in aVR” is a classic sign of a sodium channel blocker overdose, classically on board exams taught as a TCA overdose
Now, consider a Benadryl (diphenhydramine) overdose, as it is much more common than TCAs
In cases of a sodium channel blocker overdose, sodium bicarbonate will help the patient both with the sodium and the bicarbonate
The sodium serves to outcompete the toxin
The bicarb helps to alkalinize the pH and increase the amount of toxin “neutralized” by protein binding
A big thank you to Dr. Chris Belcher, APD at the University of Kentucky for sharing this case, GO CATS!
Hit me up with any questions,
Lloyd
**Looking for a dynamic guest lecture on Emergency Cardiology for your Grand Rounds? Reach out here for a lecture request by Dr. Tannenbaum**
_________________________
Lloyd Tannenbaum, MD
APD, EM Residency
Geisinger Wyoming Valley
**I’ll be lecturing in Montreal with Dr. Amal Mattu and several other friends at the Emergency Cardiology Preconference for the International Conference on Emergency Medicine in May, come say hi!**




Outstanding vignette. Informative and fun to read.
Great simplification of the toxicology and treatment. Great stuff.